Taking the Suprapubic Plunge
- Feb 9, 2022
- 6 min read
Well, this Rollin’ RN finally did it. I decided to switch up to a Suprapubic (SP) Catheter and thought I would share my experience for those considering to make the move too. Personally, I dislike any elective medical procedure, but after much consideration, I decided to take the plunge.

This account is a bit lengthy but I wanted to include all the steps for those thinking about getting this form of a urinary catheter. So, grab some coffee, sit back, and see what you think.
A bit of background information first. I opted for an SP to replace the foley catheter I’ve been using for the last 10 years. Why the change after 10 successful years of foley use you may ask. Great question. It’s mainly due to my quest to become independent. At the time of my accident, I was 48 and diagnosed as a T4 complete para. I tried intermittent catheterization to drain my bladder but quickly found out it was a difficult process to do from my wheelchair. I wanted to force fluids to reduce urinary tract infections (UTIs) but doing so made it necessary to catheterize more often. It all turned into a vicious cycle that I didn’t want to stop to do every two hours. Once I started the use of a foley, my independence soared. The foley was changed every two weeks and my husband was always there to assist. He was my teammate on this road of paralysis and did everything to reduce my struggles and I let him. Unfortunately, he passed away 3 years ago. My sister then stepped in to assist with my care as needed. It was at this time I realized I needed to work on becoming more independent in my care and the SP seemed like the next step in doing so. I decided to try the SP first before entering into a more invasive surgery such as the Mitrofanoff. Plus, there were so many positive comments in the Facebook Spinal Cord Injury (SCI) groups stating how well the SP was working for them. Still, there have been so many questions about the SP procedure that I felt a need to share my experience.
First off, I did my research on urologists in my area familiar with spinal cord injuries. I decided to ask around in the medical center rehab department. Dr. Adam Klausner at Virginia Commonwealth University Health Center was recommended. I then googled his education and experience. I trusted the recommendation but I wanted to do my due diligence to be sure he had a knowledge base to support a person with paralysis. (This is a tidbit everyone should utilize in finding a health care provider. As not all physicians are familiar or comfortable caring for someone with a spinal cord injury).
In an article written by Bradley C Gill, MD, MS titled Neurogenic Bladder, he explains the difference between the two systems of indwelling catheters.
Despite its apparent advantages, the use of a Foley catheter for a prolonged period of time (e.g., months to years) is strongly discouraged. Long-term use of urethral catheters poses significant health hazards. Indwelling urethral catheters are a significant cause of urinary tract infections that involve the urethra, bladder, and kidneys. Within 2-4 weeks after catheter insertion, bacteria will be present in the bladder of most women.
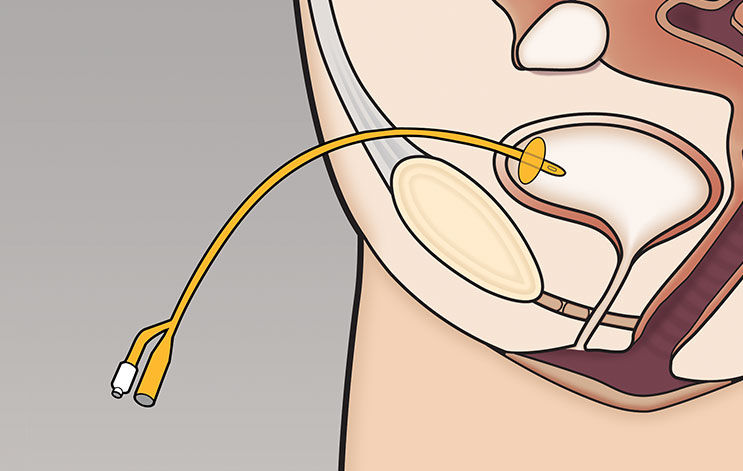
Suprapubic catheters have many advantages. With a suprapubic catheter, the risk of urethral damage is eliminated. Because the catheter comes out of the lower abdomen rather than the genital area, a suprapubic tube is more patient-friendly. Bladder spasms occur less often because the suprapubic catheter does not irritate the bladder floor as does the urethral catheter. In addition, suprapubic tubes are more sanitary for the individual, and bladder infections are minimized because the tube is away from the perineum.
Here is my account of the actual procedure:
July 16, 2021:
I scheduled an appointment with the urologist to discuss the option of an SP. I was pleasantly surprised because after some discussion his first question to me was, “do you experience autonomic dysreflexia (AD)?” Wow, shout out to this physician who knew and understood the effects of AD! My urologist explained the procedure and stated he would be injecting 40ml of Lidocaine into the bladder for numbing. He further explained that 40ml would be sufficient to numb the bladder for the procedure but not enough to set off AD. Again, impressing me with his SCI knowledge. The procedure was scheduled for September 20, 2021.
September 20, 2021, the day of the scheduled procedure:
Arrival at the medical center. My first stop was in Radiology for a bladder and kidney ultrasound. I was ecstatic to be able to remain in my chair for the testing while the renal ultrasound was done.
Moving on to the Urology department, I was taken to a room to await the urologist who reviewed the procedure again and asked if I had any questions. He also prescribed one antibiotic capsule as a preventive for infection from the procedure. Two nurses pleasantly greeted me, Sarah and Candice. Candice was a nurse training to assist with the SP procedure. She stayed with me to monitor vital signs and to watch my blood pressure in case AD started to show its ugly head. They left my foley catheter in place and injected the Lidocaine through my foley to numb the bladder. I had to wait 40 minutes for the numbing to take place, all the while Candice monitored me for signs of AD. I FELT FINE DURING THOSE 40 minutes. My legs were put into stirrups and right away I started having spasms that fought Candice. But she knew what they were, so she waited patiently until they relaxed. I was draped for privacy and to avoid getting drenched by any saline being used. Then my physician came in the room with a resident to assist. He questioned if all the staff were familiar with AD and if Nitro Paste was available, with a "yes" to both questions. Nitro Paste is used to reverse symptoms of AD but it must be closely monitored to prevent blood pressure from bottoming out.
Next, the foley catheter was removed and a scope inserted into my bladder through the urethra to visualize my urinary organs. While the scope was looking around, saline was also being pushed into my bladder. This caused ringing in my ears (an early sign of AD) and I notified the team. My blood pressure was checked and was elevated so they stopped the saline push. The ringing in my ears stopped and my blood pressure returned to normal. The two physicians then located the exact area to place the SP and did so.
A few stitches were put around the catheter to hold it in place. They also placed a 4x4 gauze pad around the catheter to absorb any blood from the procedure, and we were done. Easy peasy! So now I am sporting a 16fr, SP from my abdomen to improve my independence. Candice assisted me with redressing and getting me back into my chair.
Afterwards, I scheduled a 6-week checkup for catheter replacement.
November 15, 2021, 6-week catheter checkup and catheter replacement:
The Registered Nurse led me to a room and explained each step of the procedure to take place. She prepared the equipment and positioned me. I have a Permobil F3 power chair, so I could raise the chair and tilt it for easy access to the site. She removed the previous catheter, inserted a new catheter, inflated the catheter bulb, and flushed the tubing to remove any blood in the tubing. (Note that when doing this yourself, you want to advance the catheter during insertion until you spot urine in the tubing and stop and then blow up the bulb of the catheter to keep it in place). The urologist stopped by following the insertion process, checked on the procedure, was pleased, and instructed me to follow up in one year.
The only side effect I noticed from getting the SP done, was that my abdomen appeared more rounded than before. I think that was from the manipulation of my bowels and the placement of a foreign body (catheter) and resolved without any problems.

That’s it! My SP is now in place. Another step towards independence.
Since that last visit, this nurse has replaced the catheter all on her own! My plans going forward are to change the entire setup every 4-6 weeks.
So far all seems to be working fine. I hope that by sharing my encounter with those considering this procedure, my experience will ease any fears you may have.
I found this excellent post-procedure instruction sheet for suprapubic catheter change. https://www.mountsinai.org/health-library/selfcare-instructions/suprapubic-catheter-care
It’s all good, so keep on rollin’
Patty, BSN, RN and Roberta, RN
The Rollin’ RNs ™
References:




.png)
.png)
Comments